PA Health Policy Update for the Week of May 2-6
The following is an update of selected state health policy developments in Pennsylvania for the week of May 2-6, 2022. (Some of the language used below is taken directly from state documents.)
 General Assembly
General Assembly
The Center for Rural Pennsylvania, a legislative agency of the state’s General Assembly, has issued a report on access to mental health services in rural Pennsylvania that identifies barriers and challenges to obtaining mental health care in rural areas and offers proposals for addressing them, including expanding and funding telehealth services. Learn more from the report “Access to Mental Health Services in Rural Pennsylvania.”
The House Democratic Policy Committee held an informational hearing this week examining the opioid epidemic. Find the hearing’s agenda and testimony here.
Revenue Collection Update
Pennsylvania’s General Fund revenue collections in April totaled $6.5 billion, which is $1.8 billion, or 38.7 percent, above estimate. Fiscal year-to-date General Fund revenue collections are $4.5 billion, or 12.4 percent, above estimate. Governor Wolf issued a press release noting that April’s revenue collection was the most ever collected by the state in a single month.
 Department of Human Services
Department of Human Services
- The Department of Human Services (DHS) has announced its intent to allocate funds in FY 2022 for several classes of inpatient disproportionate share hospital (DSH) payments and supplemental payments to Medical Assistance-enrolled, qualifying inpatient acute-care general hospitals. Specifically, DHS intends to allocate $9.510 million in total funds for DSH payments to qualifying acute-care general hospitals that provide a high volume of services to the Medicaid population to promote continued access to inpatient and ancillary outpatient services and to support academic medical programs that provide integrated, patient-centered medical services; to allocate $5.917 million in total funds for DSH payments to qualifying acute-care general hospitals to promote the availability of professional medical services to Medicaid populations in less urbanized areas by supporting medical education and academic medical programs; and to allocate $40.163 million in total funds for supplemental payments to qualifying acute-care general hospitals that treat a high percentage of Medicaid patients under 18 years of age. Learn more from this Pennsylvania Bulletin notice.
- DHS has issued a Medical Assistance Bulletin to clarify its guidelines for the delivery of services via telemedicine through the Medical Assistance program’s fee-for-service delivery system. The bulletin applies to all providers enrolled in the Medical Assistance program. Providers rendering such services under the managed care delivery system should address coverage and payment questions for the delivery of services via telemedicine to the appropriate managed care organization. Find the bulletin here.
- DHS has shared presentations offered at the April 28 meeting of the Medical Assistance Advisory Committee (MAAC) by:
- DHS has posted a draft file note of the April 14 meeting of the Medical Assistance Advisory Committee’s managed care delivery system subcommittee.
 Department of Health
Department of Health
The Department of Health has issued a health alert updating its vaccine recommendations for hepatitis A and B.
The Department of Health has issued a health alert about failure to disinfect assisted blood glucose monitors between uses posing a risk for blood-borne pathogen transmission. The alert describes the problem, offers suggestions for how to prevent it, and points providers to resources for further information. Find the alert here.
COVID-19: By the Numbers
- Daily COVID-19 case counts climbed for the sixth consecutive week. The state’s seven-day average of new cases rose eight percent, from 1734 on April 28 to 1834 on May 5.
- The seven-day average of COVID-19-related deaths rose from nine on April 28 to 13 on May 5.
- The growing number of COVID-19 cases in the state has led to a corresponding increase in COVID-19-related hospitalizations, with Pennsylvania experiencing a 22 percent increase in COVID-19-related hospitalizations for the second consecutive week.
- While the number of these patients on ventilators rose 20 percent over the past week and the number in hospital ICUs rose 33 percent, the actual number of such patients remains modest in comparison to times earlier in the pandemic when the daily case counts were comparable.
- During the past week 35 Pennsylvania counties, up from 22 last week, experienced high rates of community transmission of COVID-19; two counties, one fewer than last week, experienced a low rate of transmission; 21 counties, down from 22 last week, experienced a substantial rate of community transmission; and the remaining nine counties experienced a moderate rate.
 Department of State
Department of State
The Department of State has announced that the professional licensing waivers it issued under the COVID-19 disaster declaration will begin expiring in phases starting on May 23, with all waivers scheduled to expire by June 30. Go here for a list of the department’s waivers and their expiration dates.
Stakeholder Events
Department of Human Services – Medical Assistance Advisory Committee – Managed Long-Term Services and Supports Subcommittee – May 10
The managed long-term services and supports subcommittee of DHS’s Medical Assistance Advisory Committee will meet virtually on Tuesday, May 10 at 10:00. To register to participate, go here.
Department of Human Services – Medical Assistance Advisory Committee Managed Care Delivery System Subcommittee – May 12
The managed care delivery system subcommittee of the Medical Assistance Advisory Committee will meet virtually on Thursday, May 12 at 10:00. For an agenda for the meeting and information about how to participate, go here.
Department of Human Services – Learning Network/Nursing Facilities – May 12
DHS’s Learning Network, part of its Quality Strategy for Nursing Facilities, is offering in collaboration with the Community HealthChoices managed care organizations and the Jewish Healthcare Foundation a special population webinar on avoiding hospitalizations from nursing facilities on Thursday, May 12 at 2:00. Recommended nursing home participants are admissions coordinators, directors of nursing, and social services staff. For more information about the webinar and how to register, go here.
Department of Human Services – Learning Network/Nursing Facilities – May 19
DHS’s Learning Network, part of its Quality Strategy for Nursing Facilities, is offering in collaboration with the Community HealthChoices managed care organizations and the Jewish Healthcare Foundation a webinar on the role that vaccinations, including influenza, pneumonia, COVID-19, and others, can play in avoiding hospitalizations from nursing homes. The webinar will be held on Thursday, May 19 at 2:00. For further information about the webinar and to register to participate, go here.
DHS – Office of Medical Assistance Programs – Gun Violence Roundtable – date in May to be determined
DHS’s Office of Medical Assistance Programs will convene a roundtable in May to discuss gun violence as a public health issue and to explore public health strategies that can be used by Medicaid managed care organizations to prevent and respond to gun violence. A save-the-date will be sent out in the next week or so and the managed care organizations will be given a list of questions to come prepared to discuss. An opportunity to present on current and planned initiatives, as well as challenges and limitations, will be offered to each managed care organization.
 Included in this month’s issue are articles about:
Included in this month’s issue are articles about: General Assembly
General Assembly Department of Drug and Alcohol Programs
Department of Drug and Alcohol Programs Governor Wolf
Governor Wolf COVID-19: By the Numbers
COVID-19: By the Numbers Stakeholder Events
Stakeholder Events General Assembly
General Assembly Governor Wolf
Governor Wolf Governor Wolf
Governor Wolf Department of Health
Department of Health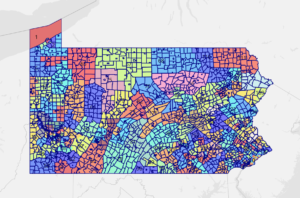 Redistricting Update
Redistricting Update General Assembly
General Assembly Pennsylvania Health Care Cost Containment Council (PHC4)
Pennsylvania Health Care Cost Containment Council (PHC4) The state’s Medicaid rolls have grown by approximately 600,000 during the pandemic, and under the terms Congress set for states to receive additional federal funding to support their Medicaid programs, the state was prohibited from re-evaluating the eligibility of those receiving Medicaid and removing them from the state’s Medicaid rolls if they were found ineligible. Once the pandemic officially ends, however, states will once again be able to review the eligibility of their Medicaid participants. In Pennsylvania today, that amounts to approximately 3.4 million people.
The state’s Medicaid rolls have grown by approximately 600,000 during the pandemic, and under the terms Congress set for states to receive additional federal funding to support their Medicaid programs, the state was prohibited from re-evaluating the eligibility of those receiving Medicaid and removing them from the state’s Medicaid rolls if they were found ineligible. Once the pandemic officially ends, however, states will once again be able to review the eligibility of their Medicaid participants. In Pennsylvania today, that amounts to approximately 3.4 million people.